Treatment of Tandem Lesions
Thank you very much Chris, what a great start, Marvin and team appreciate the opportunity to talk to you and people you might be trying to educate this afternoon. I think Chris really started off with a great presentation about the actual device and the value that it presents to carotid disease. I’m going to take a slightly different tack for those who might not know, I’m a neurosurgeon and I’m an interventional neuro specialist who does both open and endovascular procedures. I live in Buffalo at the Gates Vascular Institute and the Jacobs Institute, and what I want to educate you about is this opportunity which is currently completely unrealized.
Here are my disclosures, and I did recently sign on with Marvin’s team to advise them on their neuro strategy.
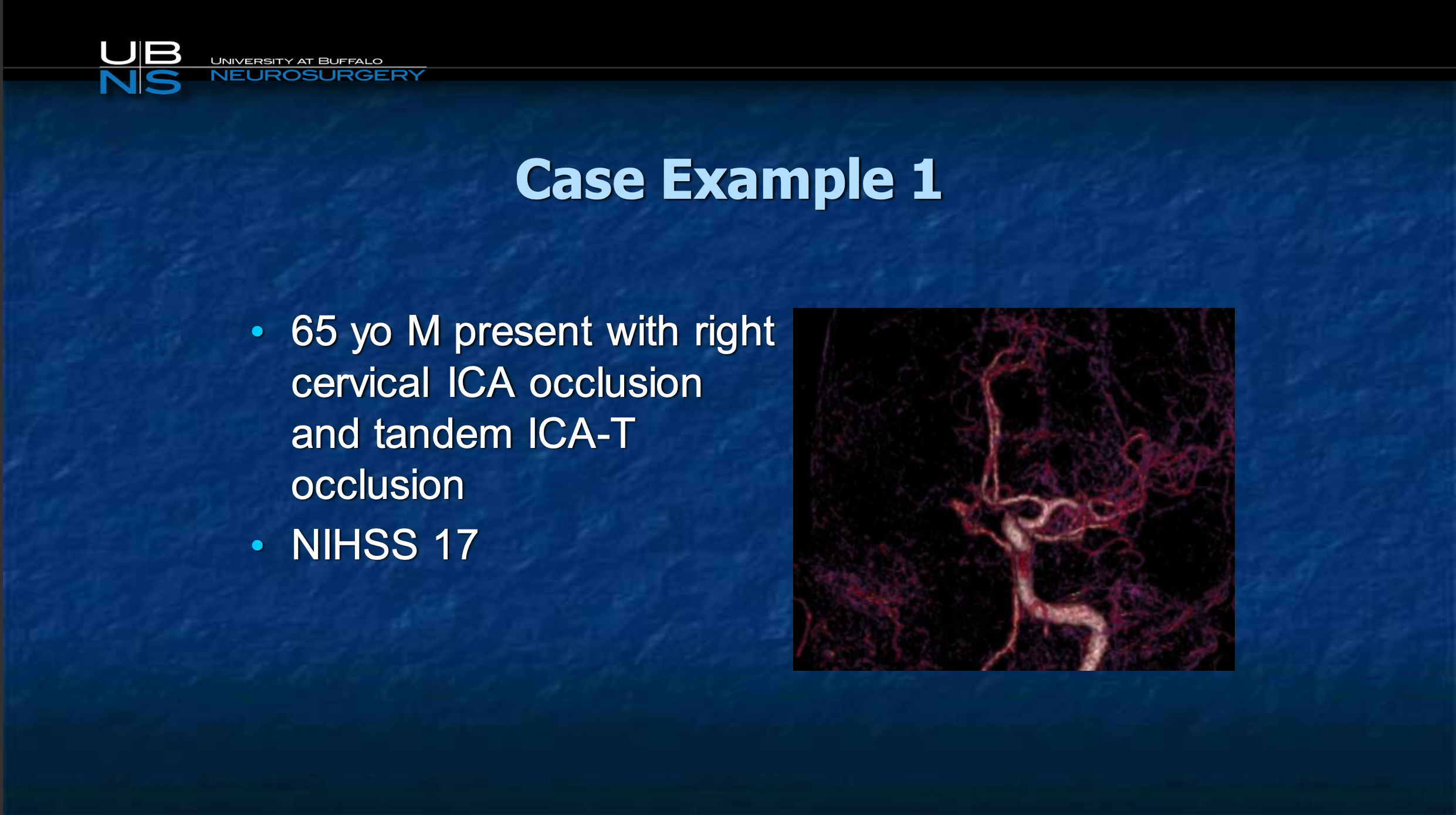
So I’ll start off by talking about a case example. It’s a 65 year old who presents with an acute cervical internal carotid artery occlusion, here’s a CTA you sort of see the vessels on the left side but you see this entire right side of the head with missing vessels. NIH stroke score is 17. For those who may not know NIH stroke scale, for five or less is mild, 5 to 10 as moderate, over 15 is likely fatal.
So, what we know with this person based on all the natural history data is that the chances of good recovery are zero, the chances of a you know dramatic recovery are 0.
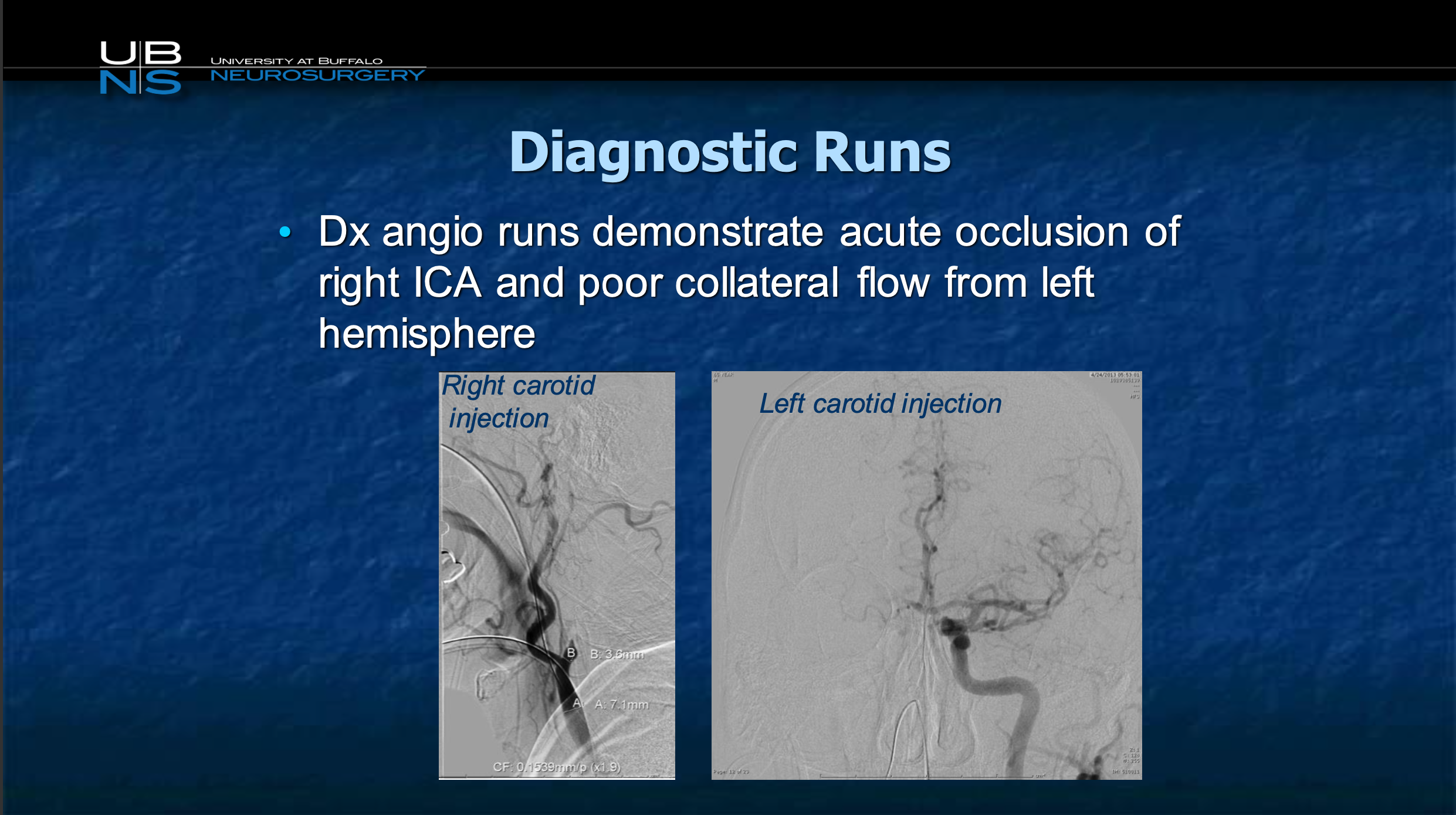
The patient is taken to the Cath lab, and here you can recognize from the pictures just shown by Chris, there’s a carotid occlusion, and there’s the flow from the other side you can see there’s really no flow going to that hemisphere.
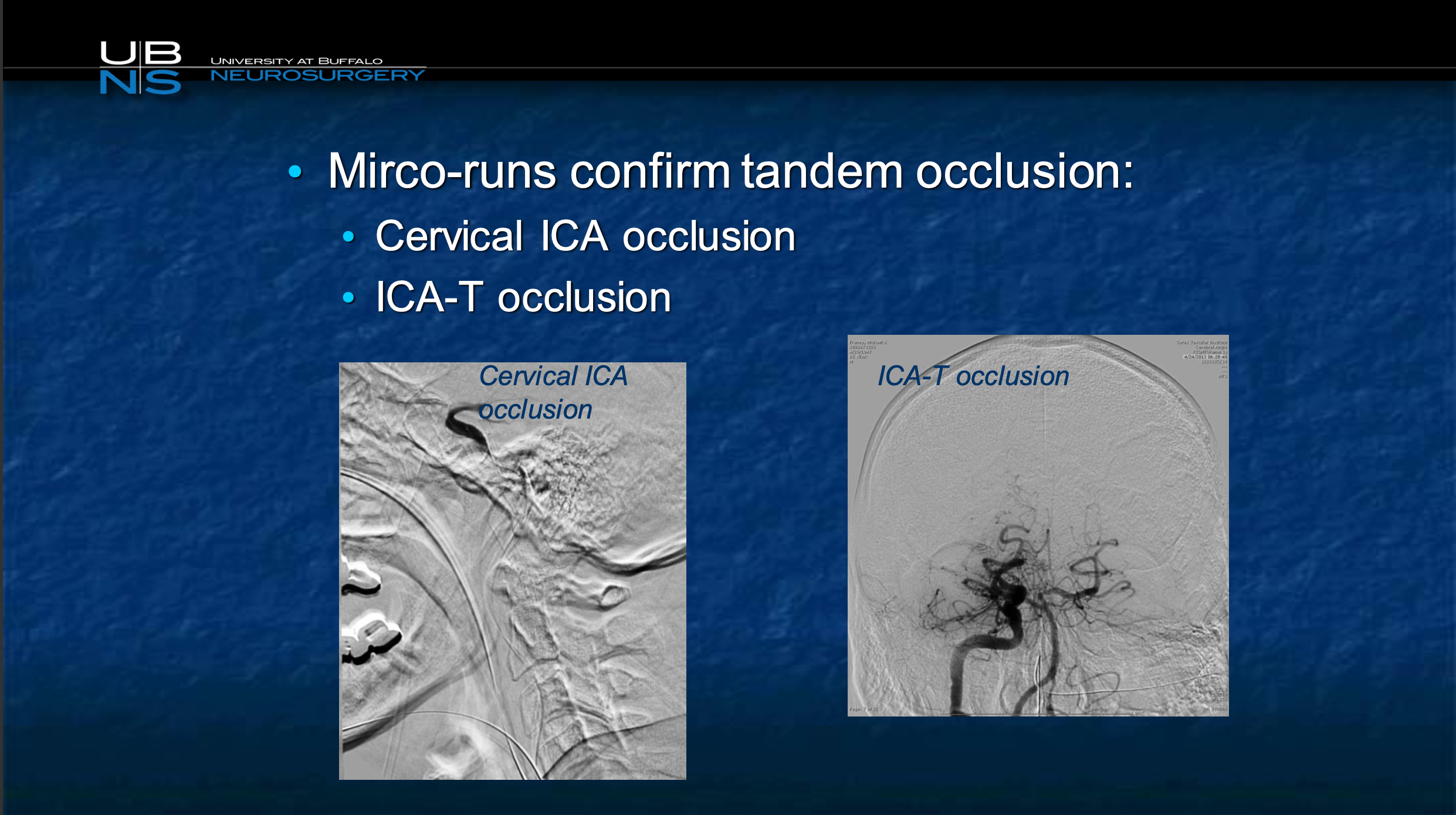
So we cross this acute occlusion, revascularized the carotid, and we realize there’s an additional lesion in the neck and then there’s another one in the middle cerebral artery.
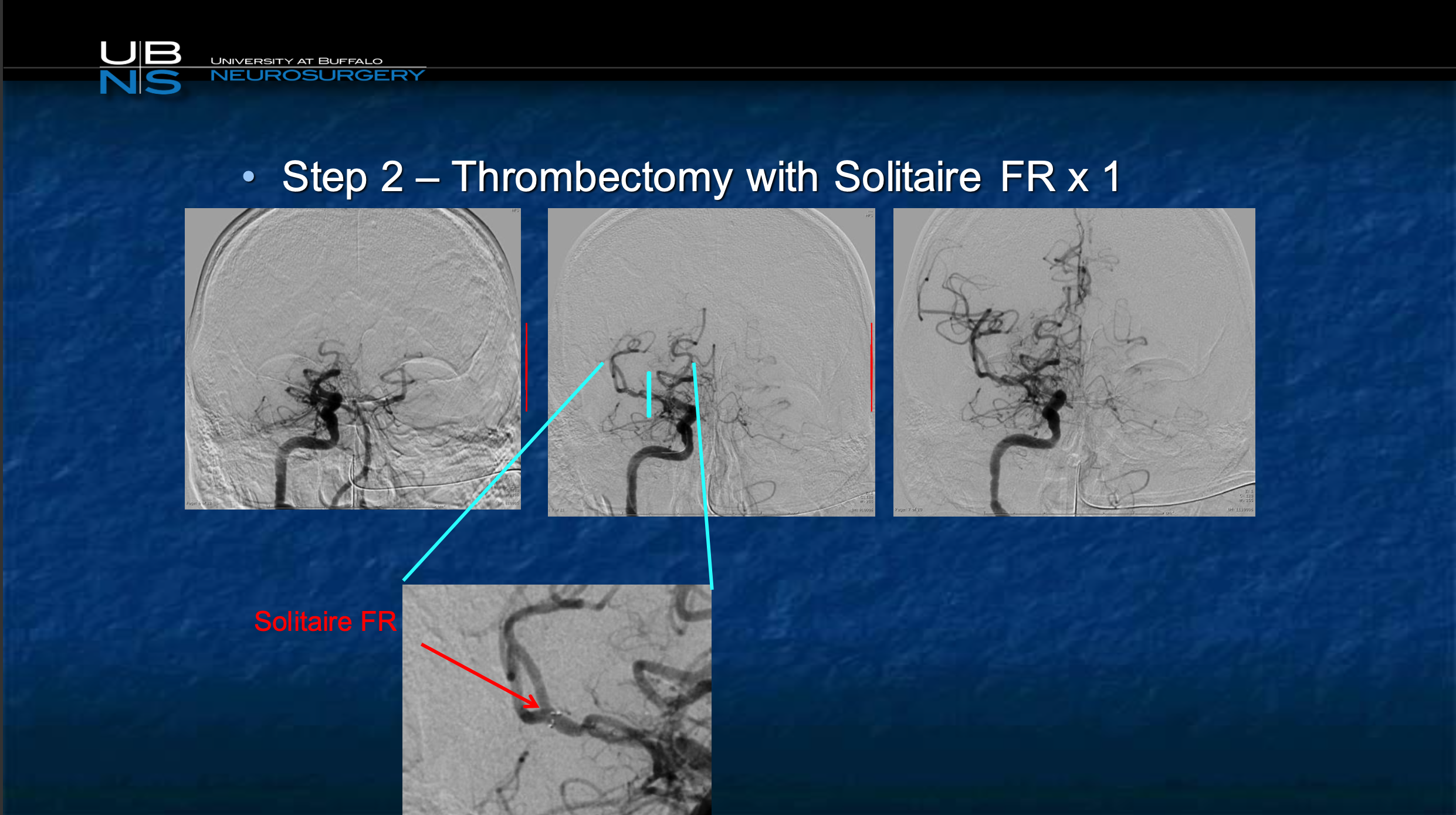
We go ahead and we revascularized that with a stent retriever, now in the end resulting in complete revascularization.
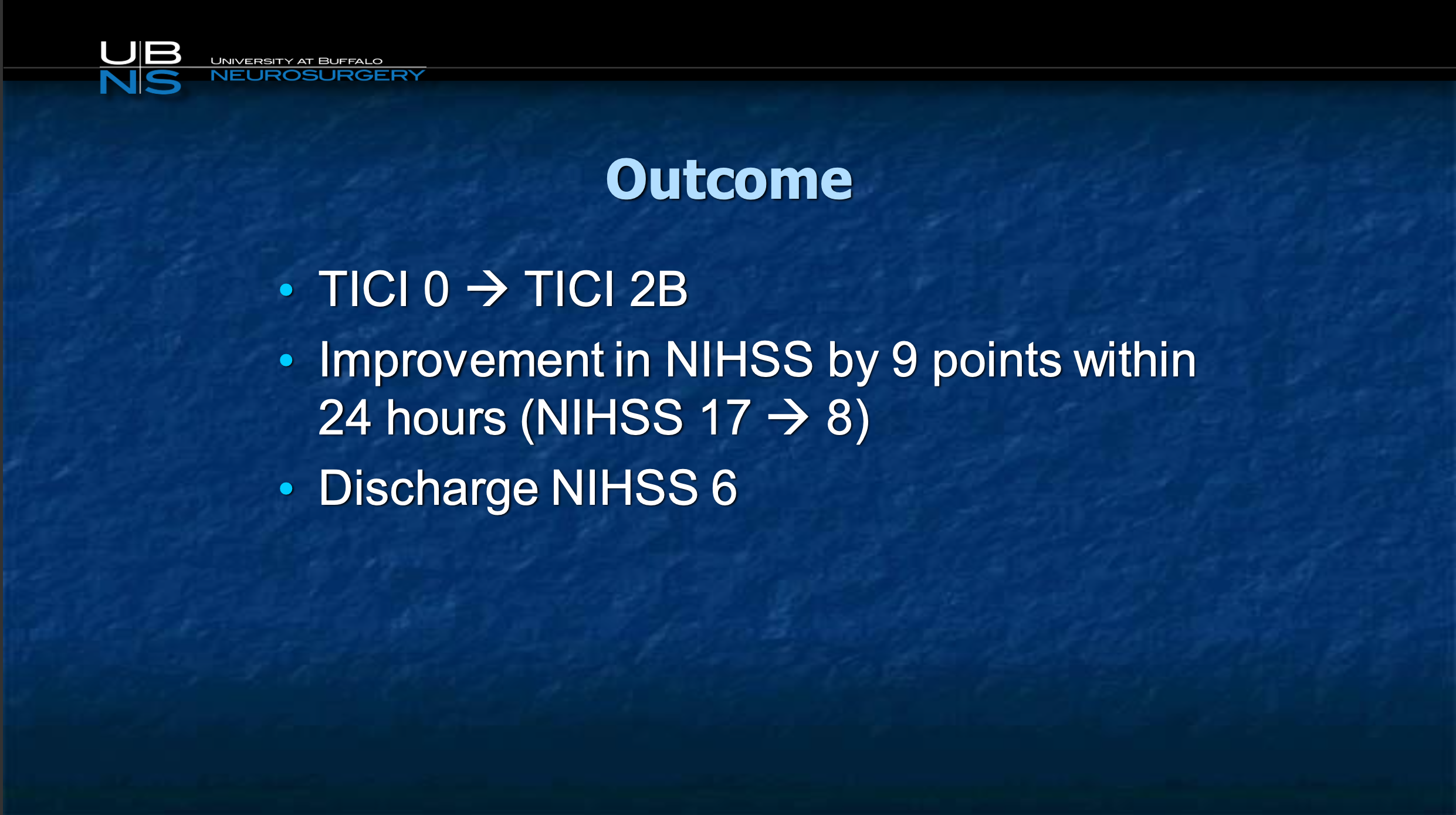
the patient improves from NIH or 17 to 8, at discharge 6, at three months 0
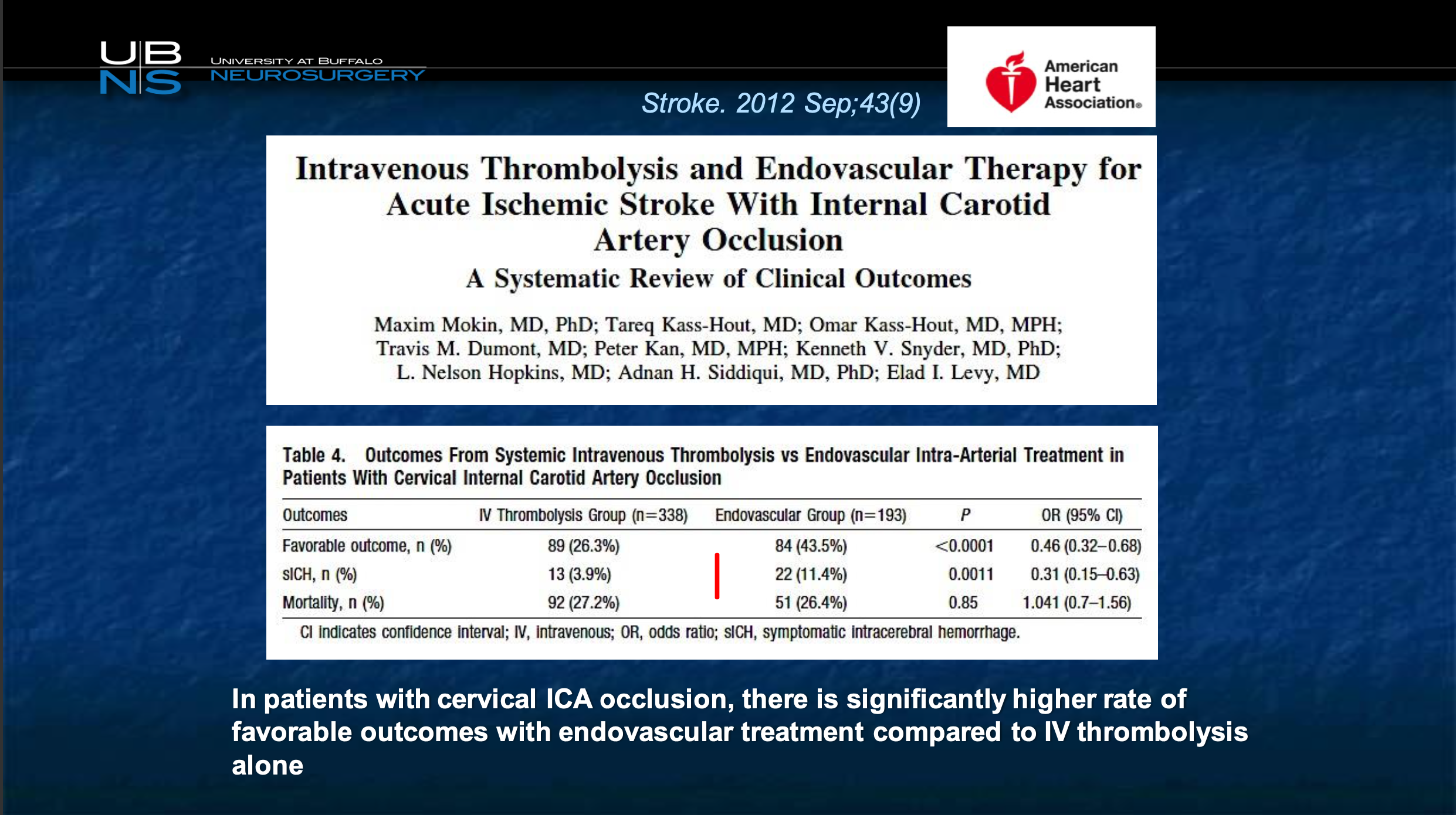
So we looked at our own data to look at patients, how patients did with carotid occlusions with thrombectomy versus with just best medical therapy particularly IV TPA, so this is not patients who didn’t get IV TPA. The significant improvement was quite spectacular, almost double the group in the endovascular achieved excellent outcome compared to those that were not treated.
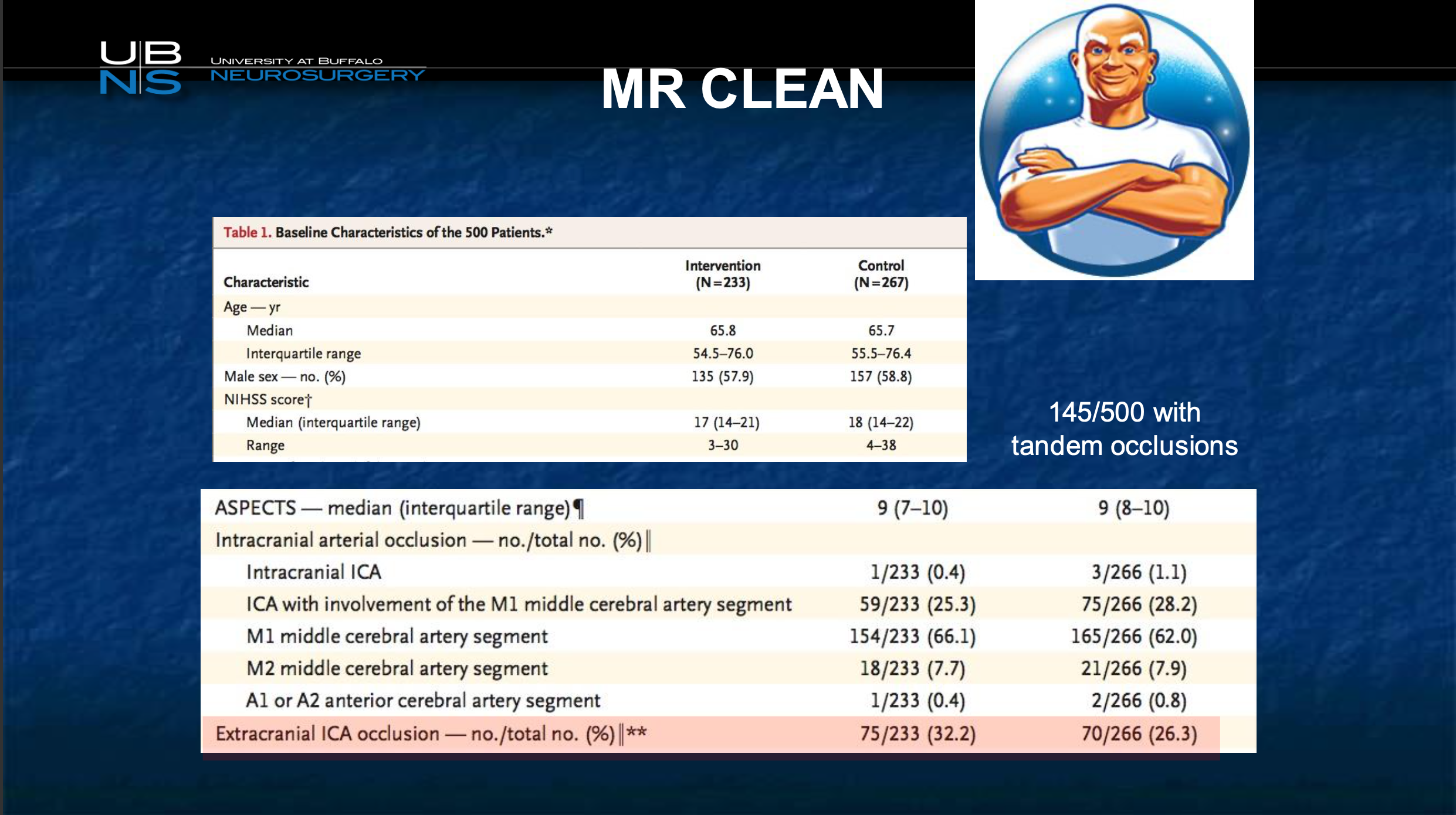
And to tell you this is not a rare group. This is a study which really started the entire revolution from mechanical thrombectomy for stroke, it was a Dutch study called MR CLEAN, and MR CLEAN included all comers who came in with a stroke and had a large vessel of occlusion. And guess- what 26% of them in the higher NIH and 32% lower NIH had a tandem occlusion, so it’s a very very very common finding in these patients. What you can see is 145 out of 500 patients had tandem occlusions so it’s a very common problem.
And what you can realize is that this is a population that was treated both in the interventional group.
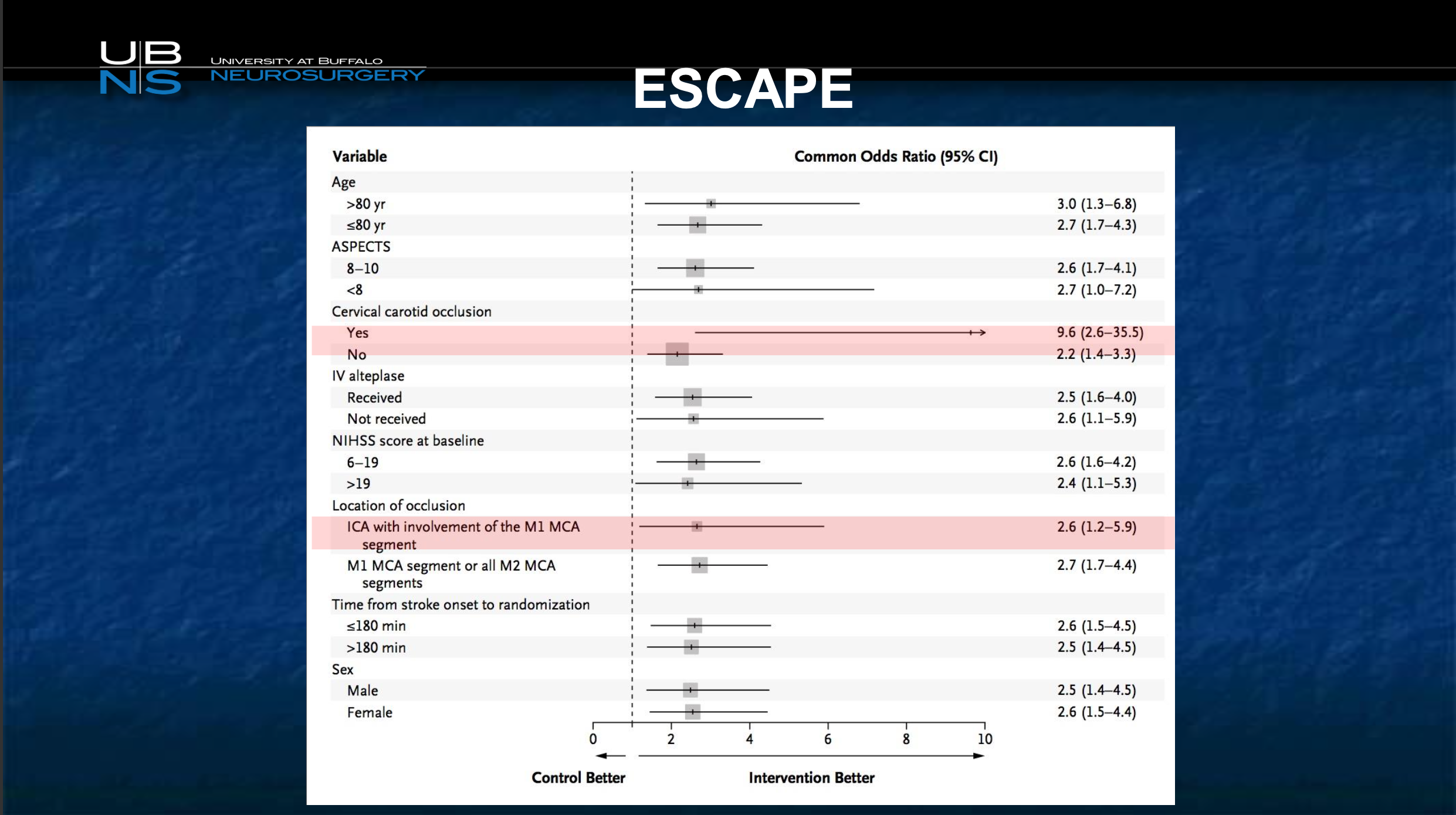
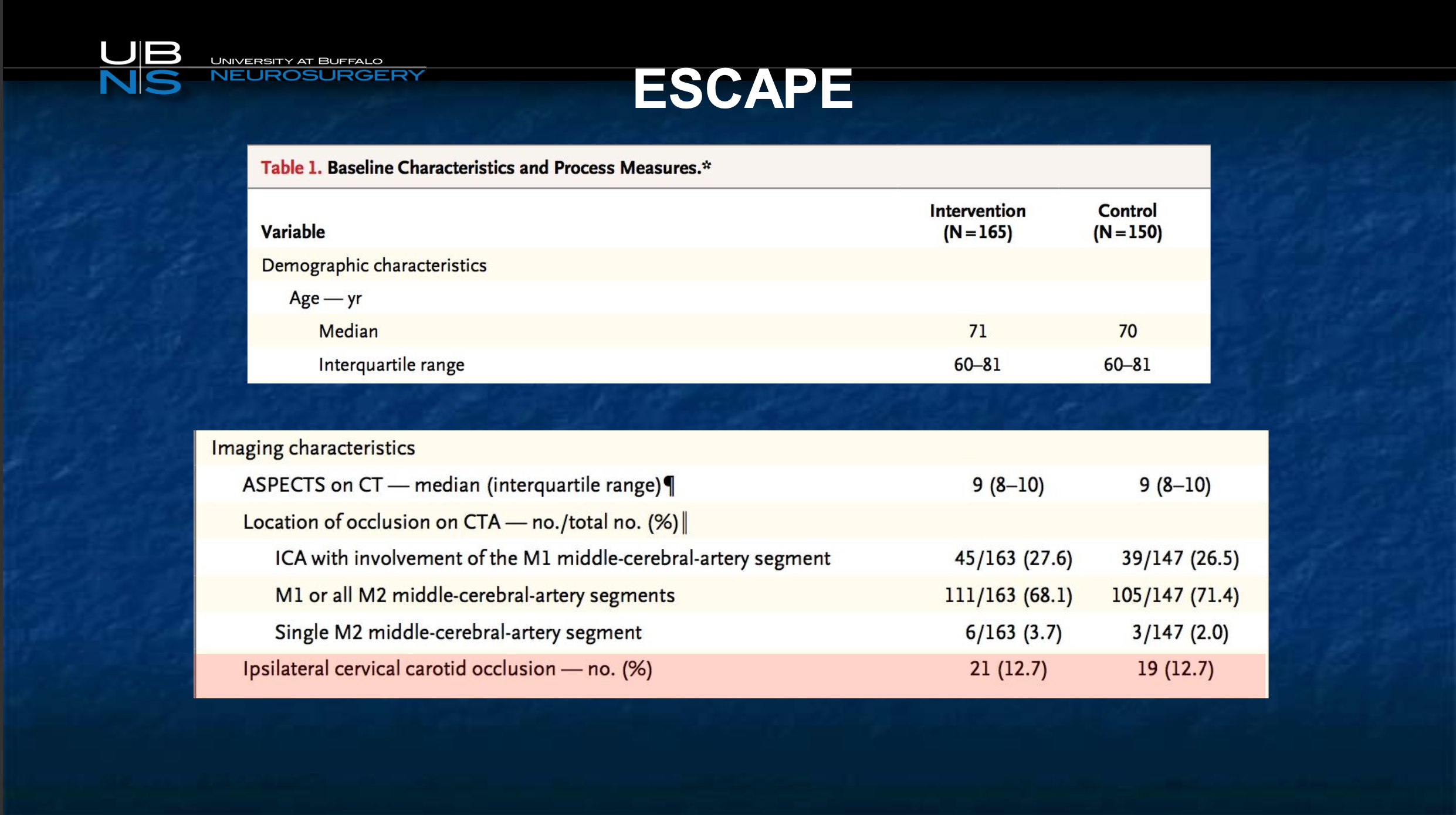
I would like you to appreciate the likelihood of good outcome, this is another trial called ESCAPE, was highest in the tandem occlusion group. So the benefit of mechanical thrombectomy, every other category whether it’s age or good looking CT scan or TPA or no TPA or severity of stroke, all those measures live out here except for one right here cervical carotid occlusion. So this is the population that you can help the most out of all the populations, and it’s not a minority. I just shared with you it’s 1/4 to 1/3 of patients and so this is really an important category.
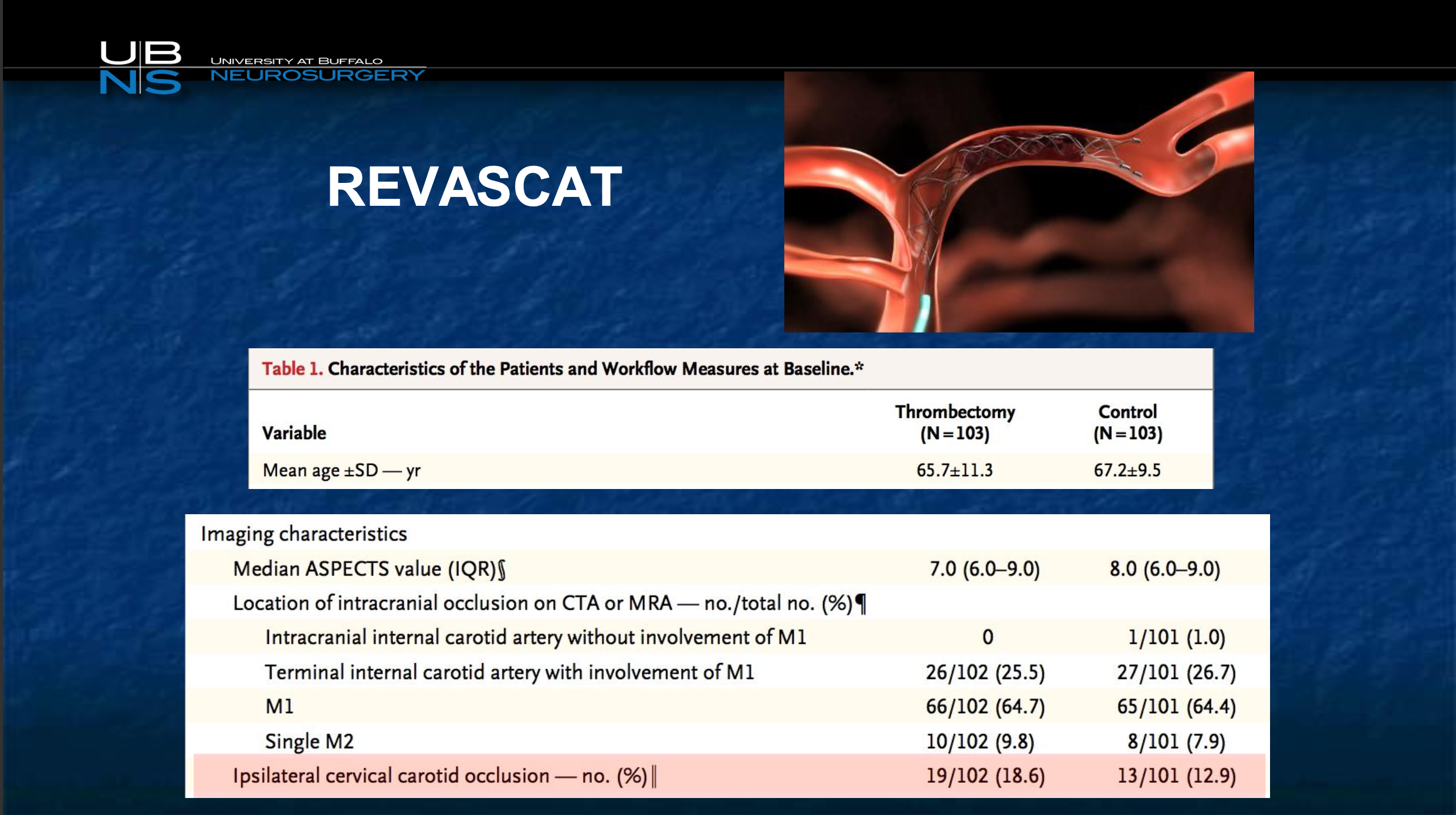
Now this is a Spanish study that was done, and by the way I’m showing you all these international studies because the FDA unfortunately has excluded all these patients from stroke trials in the United States, because there is nothing on label for this disease. So when you look at these patients, this is the REVASCAT study, almost 20% had ipsilateral carotid occlusion.
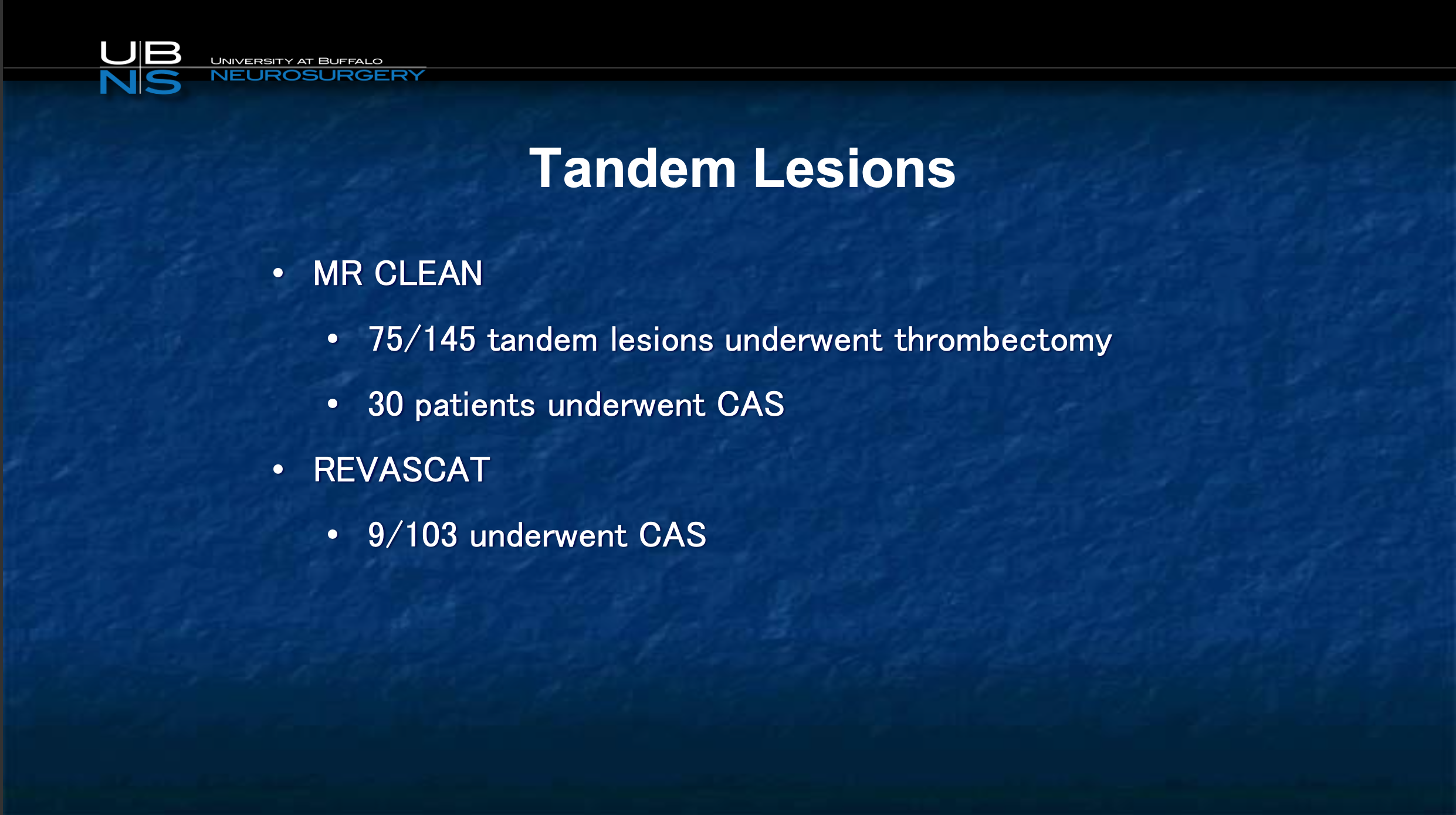
Again, when you look at all these tandem lesions. you can see that there’s value. Now, the Spanish study not a big population underwent CAS, in MR CLEAN a larger population did.
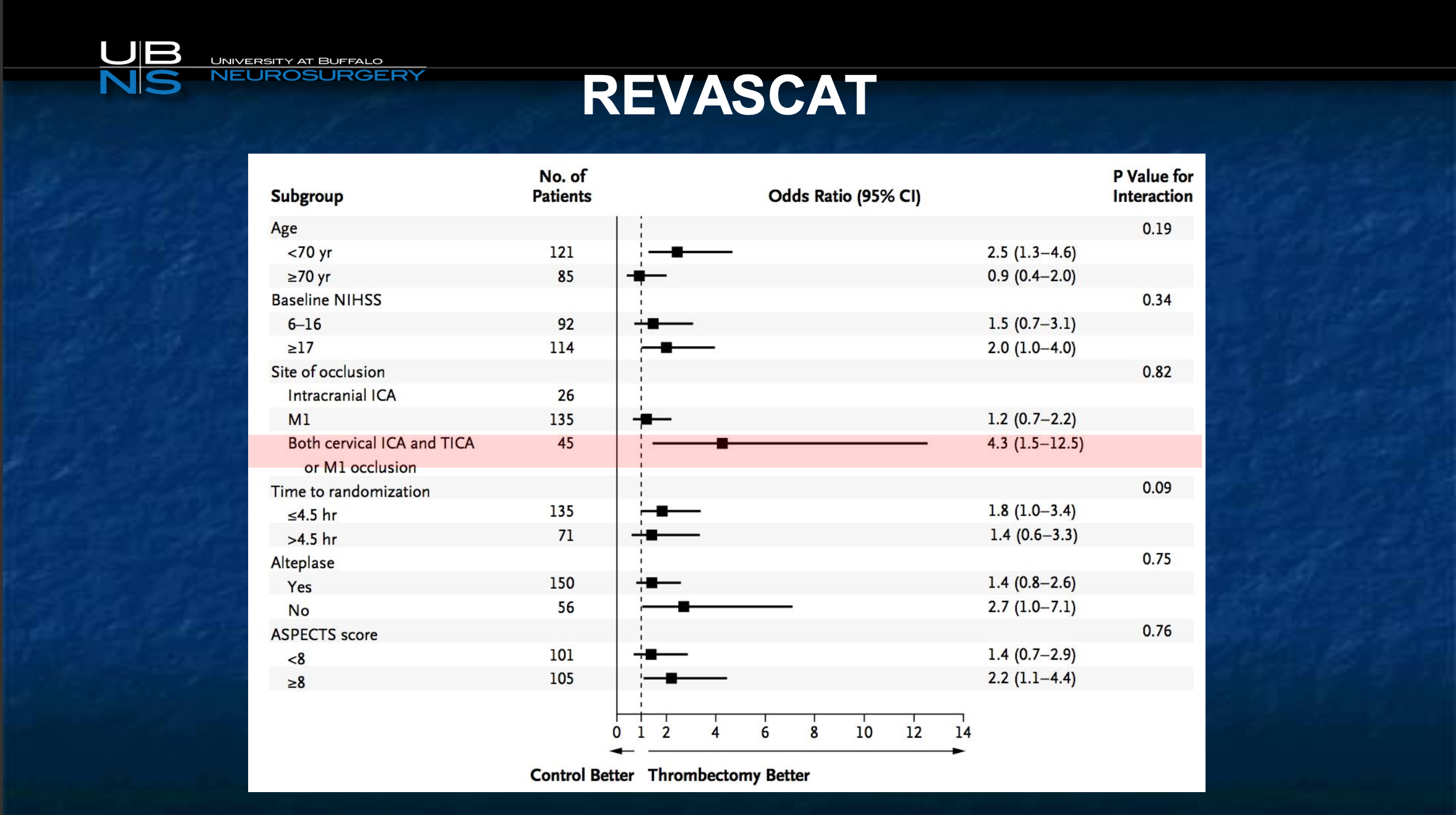
Subsequent to that, again you can see cervical occlusions are the ones that are best helped, so the question really becomes what’s the best way to deal with this.
Here’s a tandem lesion review done by my friend Frances Turjman from France.
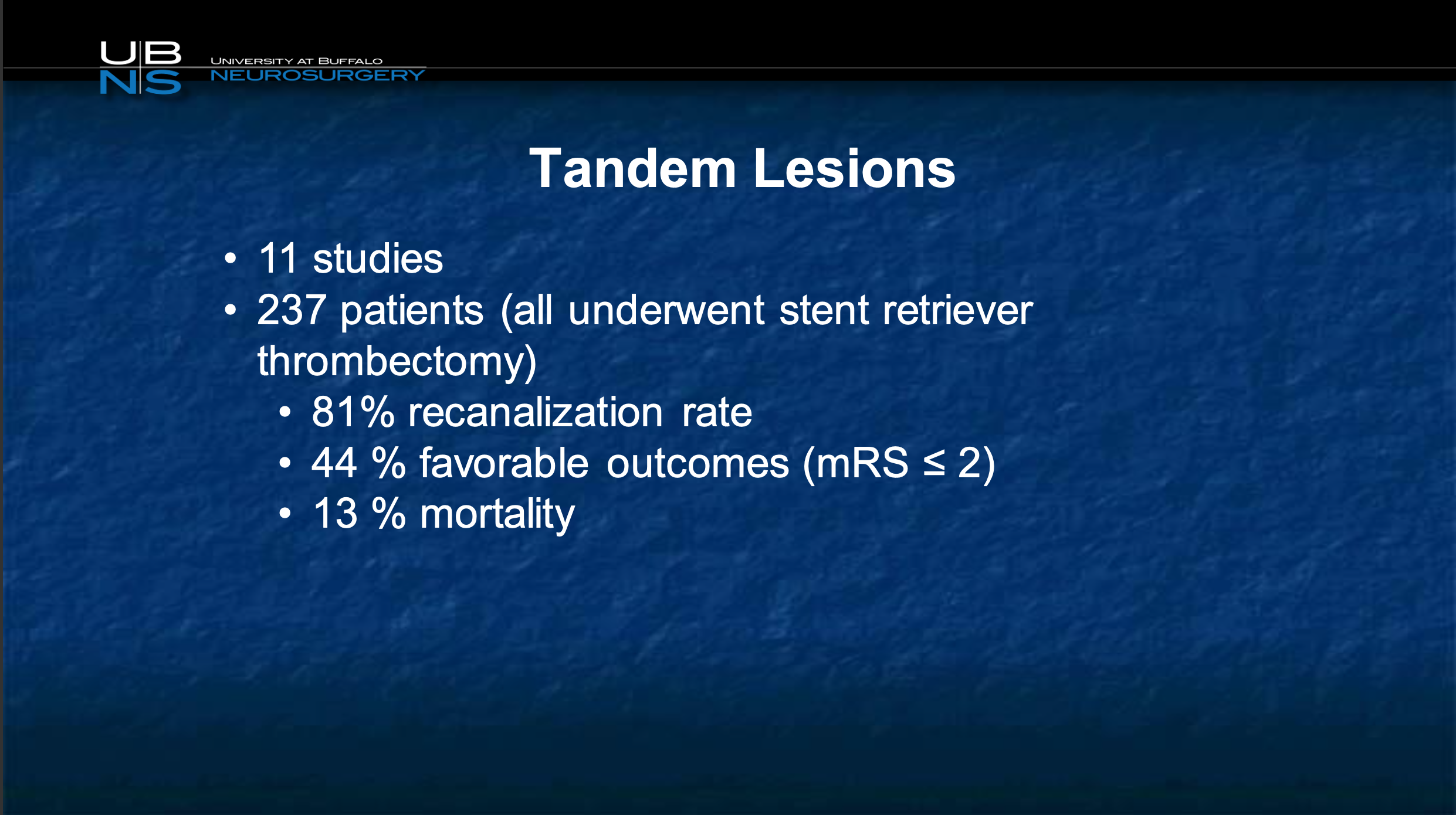
It really showed that, looking at 11 studies that were published, 237 patients, the recan rates were very good, and the favorable outcomes were just as good in tandem lesions than those who did not have tandem lesions.
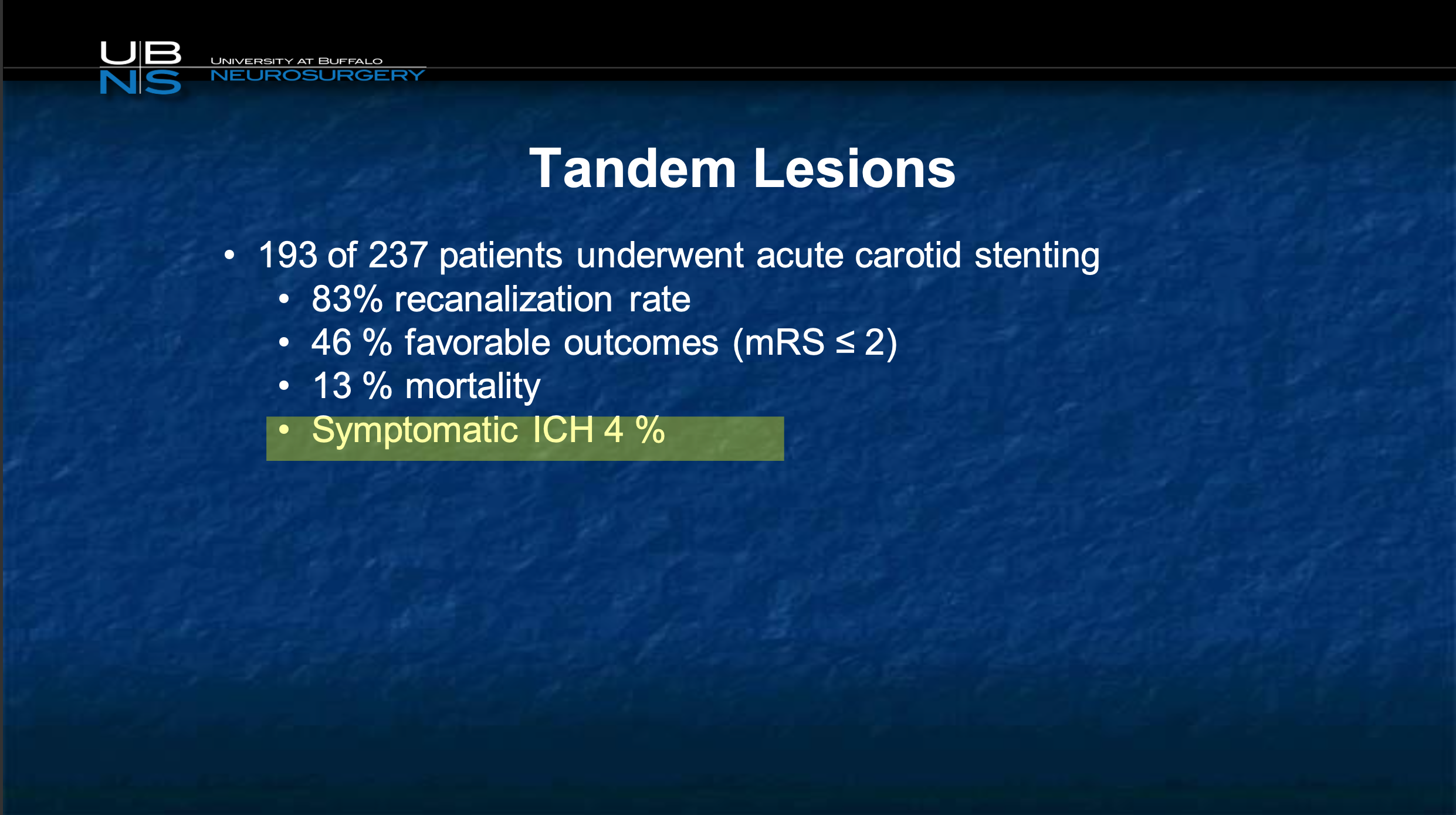
You can see in this particular series, the vast majority underwent acute stenting, and the symptomatic intracranial hemorrhage rate, that dreaded hemorrhage in the brain, was no higher than any other thrombectomy trial of only 4% and that’s well within the norm.
What’s the efficacy of tPA in ICA occlusion??
So, we know the efficacy of TPA in these occlusions is essentially 0%.
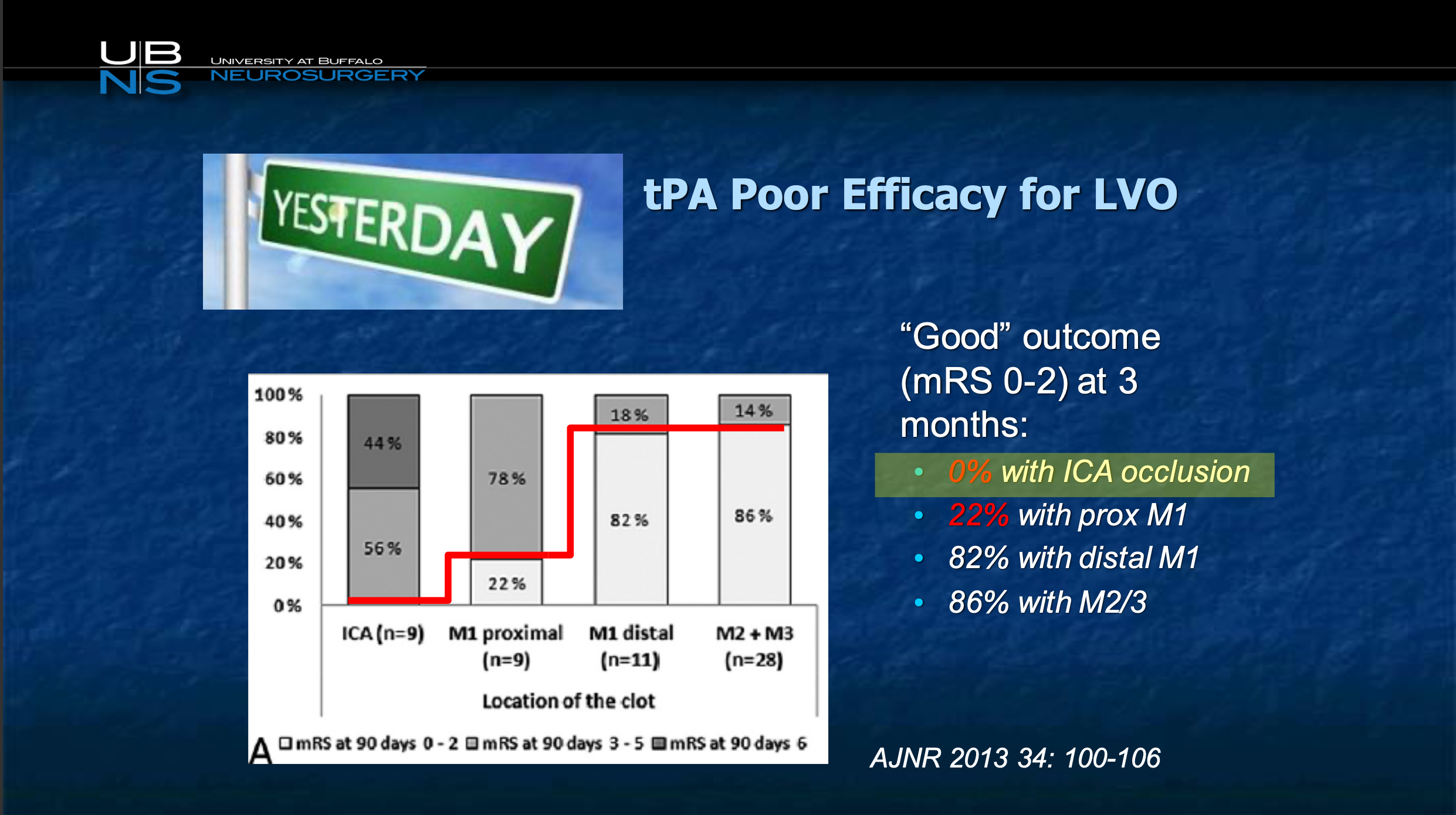
We know TPA doesn’t work in this population, so it is really hard to ascribe these patients to just medical therapy.
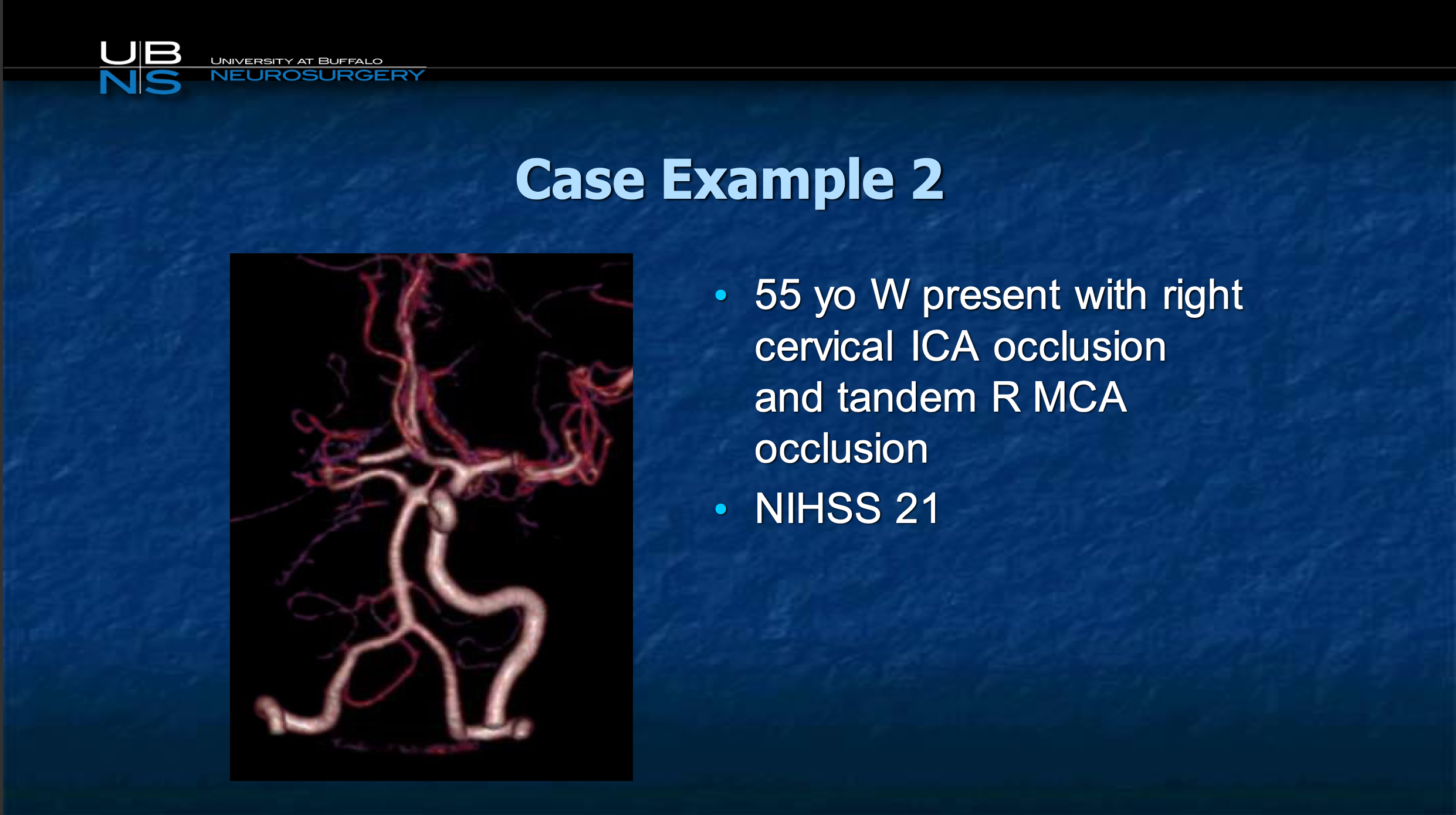
So, here’s a 55-year-old. You can again see there’s a CTA, the entire right circulation is missing. There’s the basilar, there’s the carotid, the right circulation is missing.
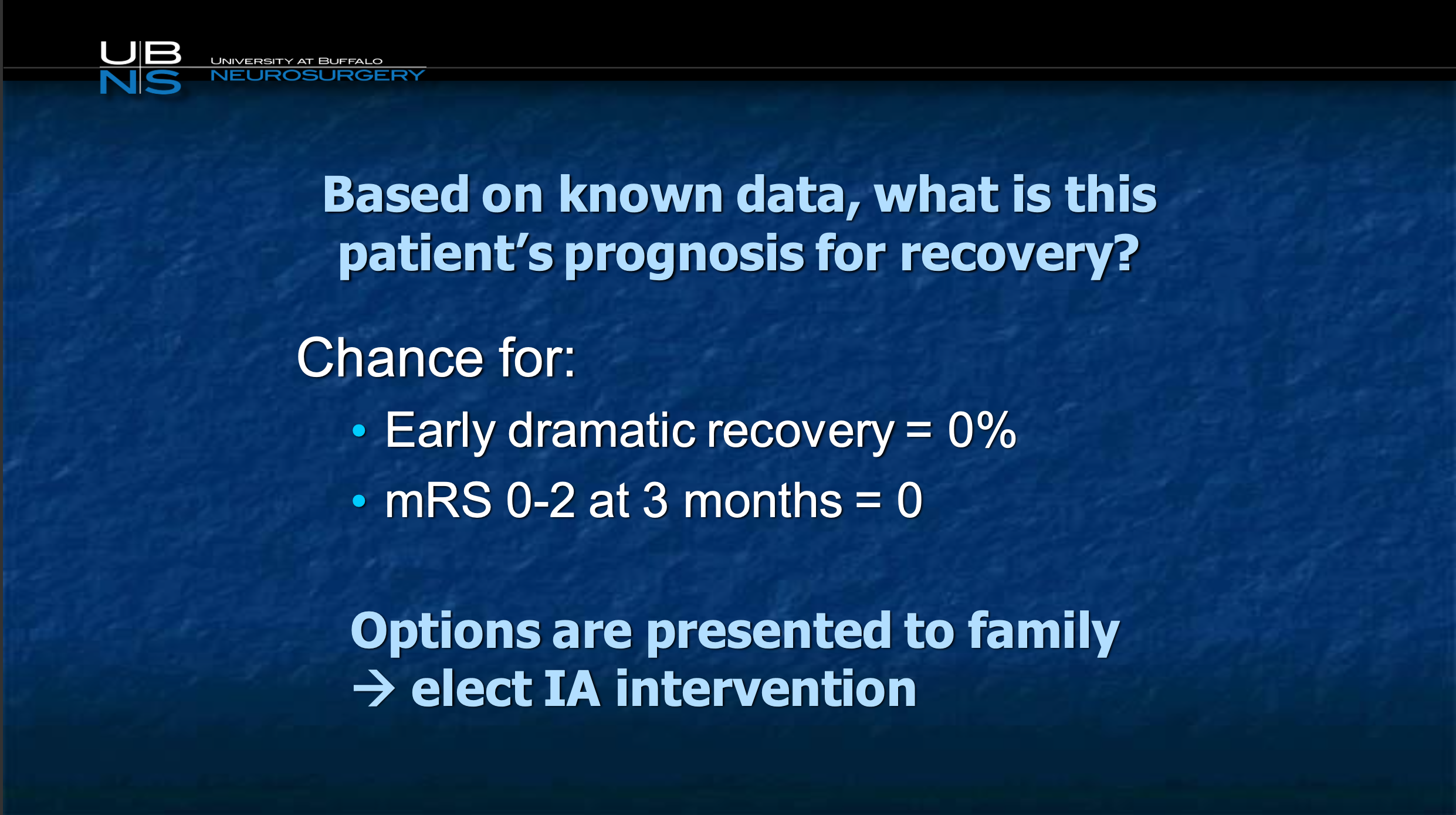
Again, chances of good outcome are zero.

There you can see there is barely nothing, you don’t even see the carotid. There’s no slow flow here, there is no flow here. But you sort of see where the carotid probably exists.
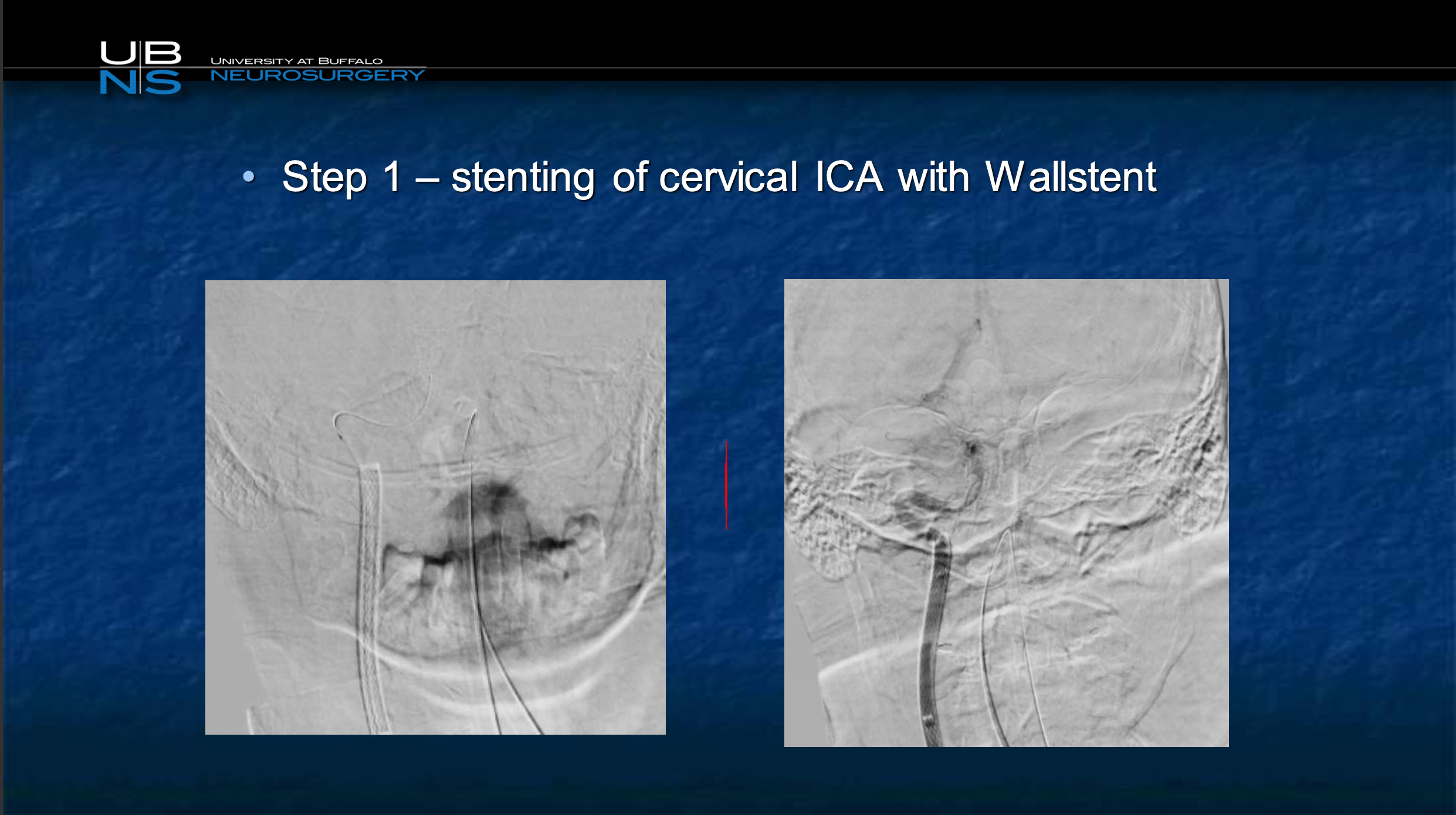
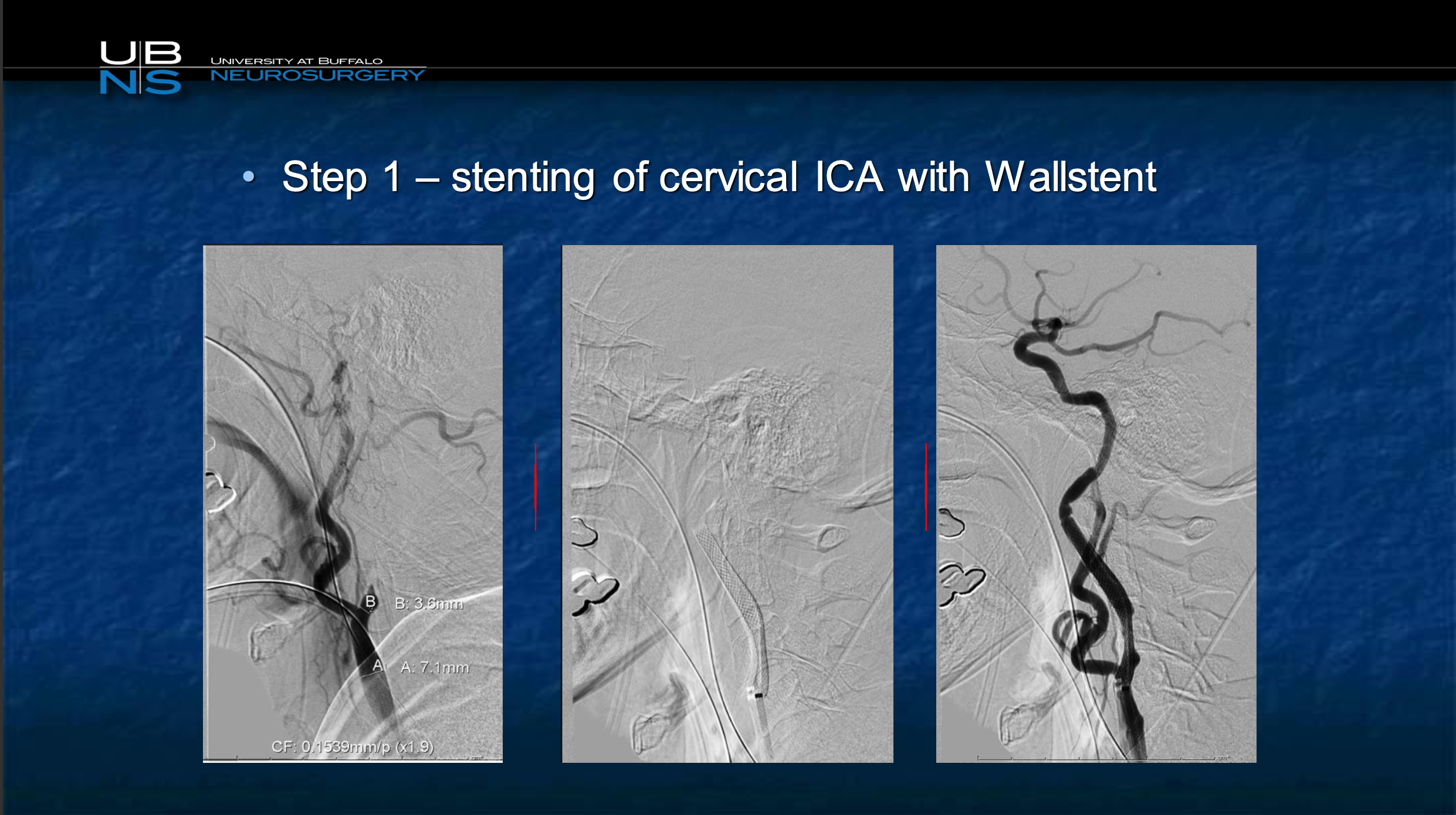
We go ahead we stent this at step one
Slide 67
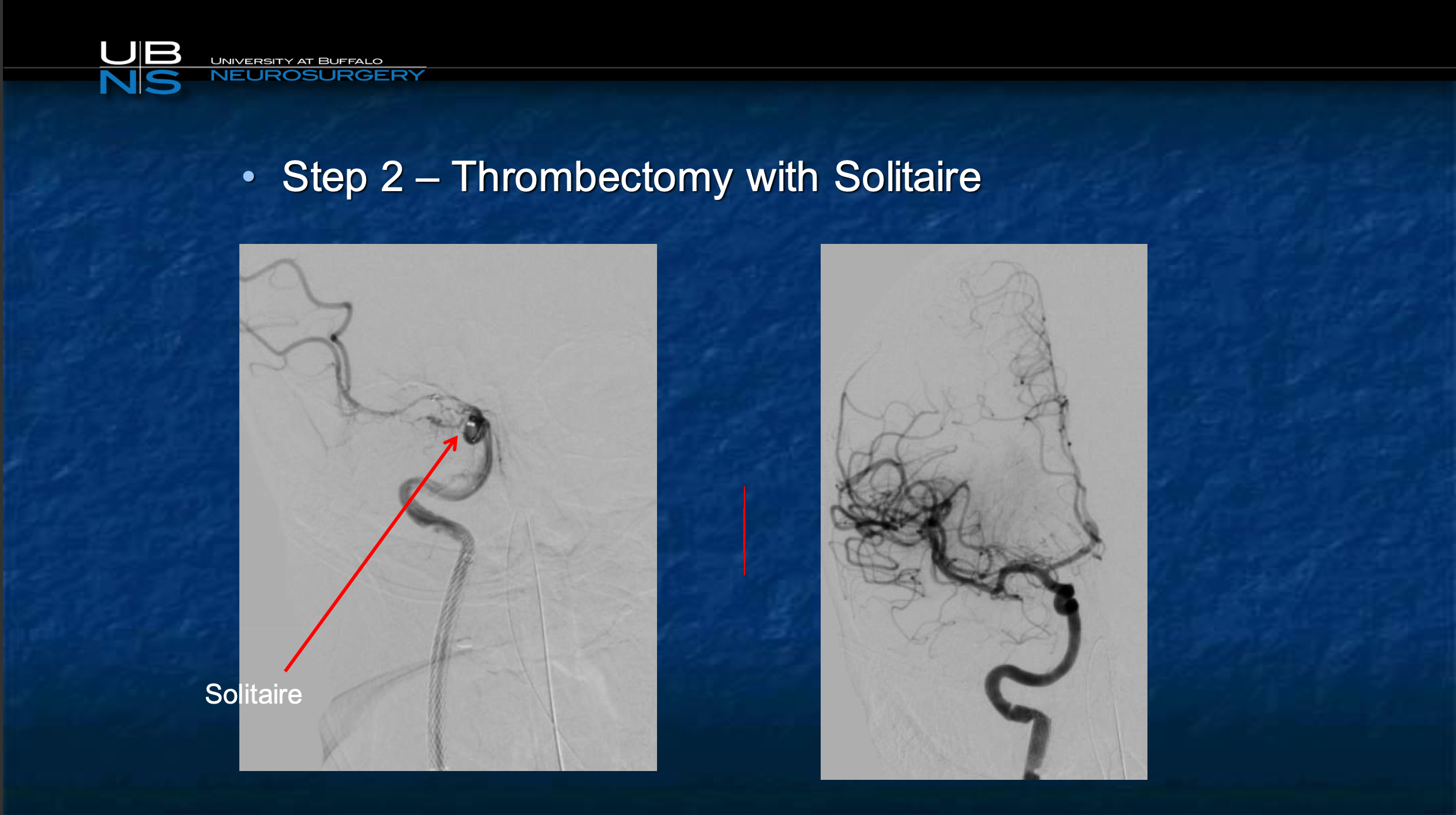
Then we go up north, and we use Solitaire. Improves NIH of 21 to 0, goes home.
So, should we stent? Do we do stenting first, do we do stenting second? What kind of stent?
I think those are all things that we still need to quite figure out. I believe I treat this as a case of a symptomatic carotid because that’s what has happened. You know, the clot’s broken off and gone up north. So, I think in the acute situation what we really do is we load the patient with Aspirin and Brilinta in the emergency room.
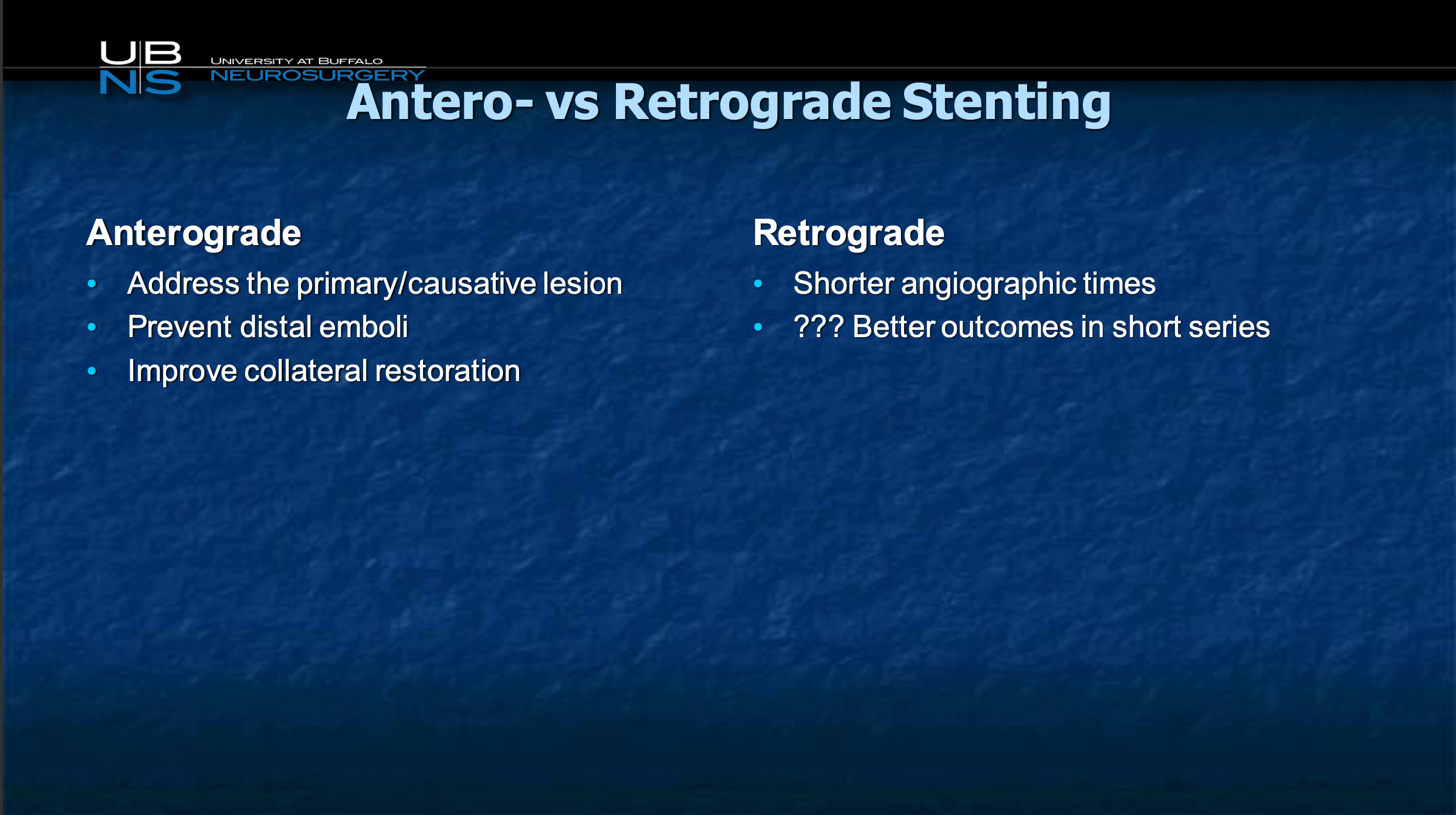
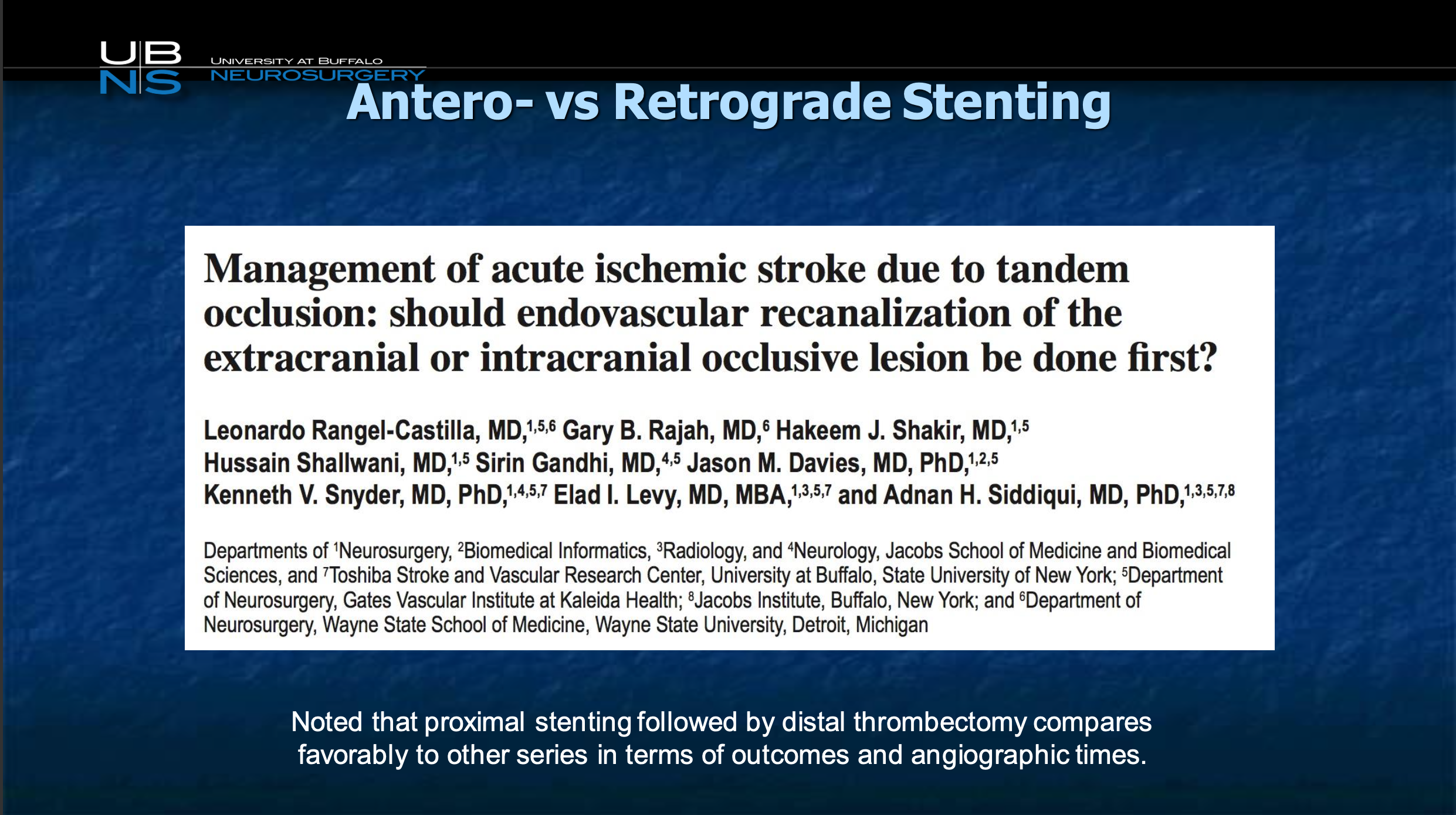
Then I like to do it anterograde, although we have looked at our data in this kind, the benefit is so good either way either it’s kind of hard to prove what it be better. I’d like to address the primary causative lesion, especially if we had a stent on the shelf that we could use for this, such as CGuard that I know that I could go ahead and plasty and not worry about this plaque shoving off stuff as I go up north and improve collateral circulation. Other people believe that maybe open the head first and on the way out open this. Again that’s an open discussion.
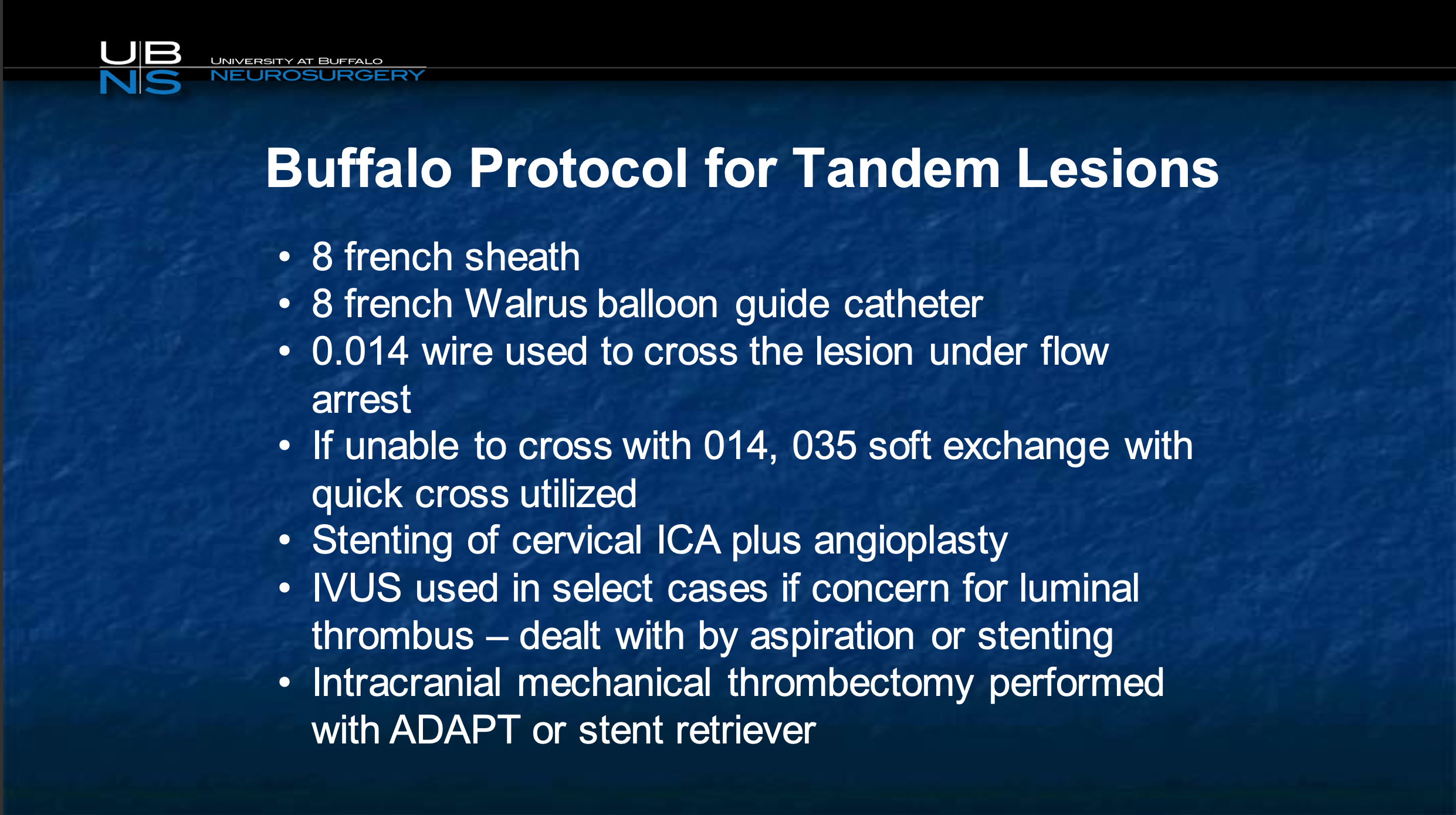
But what I like to do is use a balloon guide catheter, and we showed that there’s actual flow reversal with just a balloon guide, we don’t need to use a MoMA. We crossed the lesion and then we go ahead and plasty and stent the carotid first. If we are concerned, and then we aspirate aggressively, if we are concerned there may be still a goober we can do IVUS but we typically do directly deflate the balloon, go through the stent with the balloon guide, inflate it on the other side and do what we need to do intracranially to get good results.
So, here’s a quick video to show you that this is a critical carotid. You can see there is very very slow flow, it’s not going up north, looks like a pseudo-occlusion. So this is an older case and I’ll show you this is a MoMa device, this is something that Chris really brought to our attention along with Nick. And what you can see is we get the carotid open but there is intracranial occlusion up north in a very slow fashion. So, we inflate the balloon in the external, we inflate the balloon in the common and bring in a stent and go ahead and deploy the stent. And once the stent is in place, we still have the occlusion, so we now switch around and deflate and we put the guide catheter through. So this is why I switched away from MoMA, Chris, because it requires me to switch the guide around so with the walrus I don’t need to do that. So you can see I still don’t have intracranial flow because there is a thrombus, so now what I do is I go up with my aspiration catheter up top and cross into the middle cerebral artery and then once I have that there I’m deploying a stent retriever right there and once the stent retriever is deployed I aspirate back and I pulled this back together. And there is a run, and we have completely restored flow. This is the final run it shows complete restoration of flow and almost always you can guarantee when you see this that you’re going to have, and there’s your carotid cervical run.
So, and you know I’m going to sort of skip this to just show you, make the point that, the problem in this case is when you have a case like a tandem occlusion, you don’t have enough time to put patients on long term dual antiplatelet therapy. By the way, here’s another case of a profusion defect in the middle cerebral artery. This is the person who has got reduced flow, volume is up, you don’t open them up now he’s going to have a lot of dead brain. There’s a CTA showing you the MC occlusion and there’s critical stenosis of the carotid as well. So what do we do? We go ahead stent the carotid, we use a distal filter in this particular instance because we have a clear lumen that we can see. The stent is being deployed so we snap the thrombus in its location. Imagine if we had a stent that would actually trap that thrombus completely rather than have it protrude through the tines. The stent is being plastied, and once we have that then we again aspirate through. And there’s the MC occlusion and we go across there is the micro catheter being placed in the middle cerebral artery, and once we have that we put a stent retriever, and once we have the stent retriever in place we pull it back and we get complete recanalization of the middle cerebral artery, before and after. So the big challenge with devices here when it’s acute stroke is what are we going to do about dual entry platelet therapy number one, and number two, how are we going to protect this ruptured plaque from continuing to send plaque up north. I think both those issues are very well addressed with the CGuard device because it’s an open cell, low metal surface area device so you don’t need as aggressive anti platelet therapy as with a higher metal density device, and second the mesh allows a lot better plaque prolapse after the procedure, so again I look forward to and hopefully Marvin will be convinced that stroke is something that he needs to pursue, and I hope you guys will help them go in that direction. Thank you